You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Coronavirus
- Thread starter Hekate
- Start date
The Thriller
Well-Known Member
Another high today for Utah. Good times.
yep. Saturday for the last 2 months:
May
5/2: 189
5/9: 184
5/16: 155
5/23: 203
5/30: 269
June
6/6: 546
6/13: 404
6/20: 646
I expect us to have most days full of 500+ cases this week and topping 800 at least once. We’ll be hitting 1,000+ new cases daily in July.
Red
Well-Known Member
Strolled out to Harmons today and purposefully counted masks vs. non masks. Was 6 masks to 26 non-masks.
Drove home and saw crammed splash pads, team sports, people closely dining, etc. Social distancing is effectively done-zo here.
It's just irritating. I hate wearing masks, but do it to protect myself and others. Hate not going to places to eat, but do so to protect myself and others. Problem is that people are effectively over it.
What's worrisome to me is that the positive % metric is a leading indicator of an outbreak. That number has effectively doubled recently.
Wearing masks inside establishments is still mandatory in Rhode Island. To be at all as effective as possible, wearing a mask has to be an “all for one, one for all” proposition. I am wearing a mask to protect others, not myself, and others are wearing masks to protect others, including me. Hence, one for all, all for one. It does me little good to enter a supermarket wearing a mask, if half the people inside are not wearing masks. But it’s still mandatory here, and one is not allowed inside any establishment without a mask. For the most part, we have taken COVID-19 very seriously in RI, but we were sandwiched between states with the highest numbers of infections and deaths. And that fact will wake ya up quickly.
The Thriller
Well-Known Member
“These numbers are sobering. For three straight weeks now our cases have been increasing at a rate that isn’t sustainable. We are at risk for overwhelming our hospital capacity, which could result in Utahns not getting the medical care they need. The only explanation for this increase in cases is that we are experiencing a real and a dramatic rise in the spread of COVID-19 across our state,” Dr. Angela Dunn, epidemiologist with the state health department, said.
https://www.deseret.com/utah/2020/6...643-new-cases-no-new-deaths-hospital-capacity
The Thriller
Well-Known Member
Ummmm
this sounds criminal
this sounds criminal
Avery
Well-Known Member
Ummmm
this sounds criminal
But he's kidding!
Well, not really. Using this theory, we could reduce suicides in the US down to zero if we simply counted them as births instead.
Another low today of 267. Lowest since March 23, three months ago. Again, you can say this is a weekend, but there have been 26 weekend days since then with none of them being that low. Tomorrow’s numbers will again be lower before ticking up a little bit Tuesday.
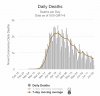
Obviously, one could appeal to the past few days having increased cases. However, the deaths have continued to steadily decline for the past two months, independent of the fact that incidence of new cases hasn’t dropped. While we’ve had higher numbers the past few days, we’ve also set daily records for the quantity of tests administered, and the US is testing more than anyone else is. True, our curve with relation to new cases looks worse than other countries’, but our death curves look the exact same as all those other countries.
But nobody’s talking about that.
fishonjazz
Well-Known Member
Contributor
2018 Award Winner
2019 Award Winner
20-21 Award Winner
2022 Award Winner
2023 Award Winner
2024 Award Winner
2025 Award Winner
Nobody's talking about that? Isn't that all you have been talking about?View attachment 9484
Another low today of 267. Lowest since March 23, three months ago. Again, you can say this is a weekend, but there have been 26 weekend days since then with none of them being that low. Tomorrow’s numbers will again be lower before ticking up a little bit Tuesday.
Obviously, one could appeal to the past few days having increased cases. However, the deaths have continued to steadily decline for the past two months, independent of the fact that incidence of new cases hasn’t dropped. While we’ve had higher numbers the past few days, we’ve also set daily records for the quantity of tests administered, and the US is testing more than anyone else is. True, our curve with relation to new cases looks worse than other countries’, but our death curves look the exact same as all those other countries.
But nobody’s talking about that.
Sent from my ONEPLUS A6013 using JazzFanz mobile app
Yes. Is this something you already been hearing elsewhere?Nobody's talking about that? Isn't that all you have been talking about?
Sent from my ONEPLUS A6013 using JazzFanz mobile app
The Thriller
Well-Known Member
Yes. Is this something you already been hearing elsewhere?
Why do you think the deaths are going down? Has the virus mutated to be less lethal? Are we getting better at treating it? Or have the weakest serving in vulnerable positions already been killed?
Why do you think the deaths are going down? Has the virus mutated to be less lethal? Are we getting better at treating it? Or have the weakest serving in vulnerable positions already been killed?
I'd have to look at case/death rates by age around the globe, but my first guess would be that I think what we were concerned would be a weakness might actually be a strength - we have most of our extremely elderly isolated from most of society.
I’m not entirely certain, but I think there are a handful of variables that may be relevant:Why do you think the deaths are going down? Has the virus mutated to be less lethal? Are we getting better at treating it? Or have the weakest serving in vulnerable positions already been killed?
- Most deaths were in nursing homes. There was less lead time initially getting this shut down, and by the time it started spreading it wasn’t able to be contained in those settings as well is it can now. I have my own story regarding this that I’ll share more on when this is all over, but it was a very scary situation going for over a month that I had no relief from.
- In relation to above, people are self-selecting their exposure levels, and if we had more data on the demographics, I’d suspect the age distributions of those infected would trend to lower ages over time.
- We’re simply catching more. We don’t know what the true incidence is or has been, but the best available way we can capture that is through confirmed cases. How accurate # positive each day truly correlated with its prevalence is unknown. Could it be that right now we have a drastically lower prevalence but it appears larger because of increased capture by testing? Perhaps in part. Some places the % of tests positive has increased, though, so it’s hard to say, but it’s also hard to determine what levels of selection bias may be introduced in testing and how that has varied both over time but also geographically, so it’s a huge question mark.
- There’s a theory that perhaps it’s mutating. I guess that could be true. That could be good, but could also be bad. It’d be kind of odd, though, just in my opinion.
- There’s another theory that the viral load people are exposed to is currently less, largely as a result of masks and social distancing. I’m not certain how much I’d buy that, but it’s possible. It could explain why some young healthcare workers got fairly sick and/or died, but it’s also hard to determine if that belief is a result of availability bias as those deaths would receive more coverage (how many nursing home patients can anyone name who have died?).
- There could be an iatrogenic effect. In the face uncertainty and the unknown, there’s a huge bias toward heavier intervention. It’s a result of feeling powerless. It’s not entirely inappropriate, though. In the middle of a pandemic, it’s reasonable to tolerate throwing some things at the wall that you otherwise wouldn’t under normal circumstances. There was a huge emphasis on ventilators. A lot of patients were apparently tolerating hypoxia clinically but the hypoxia can be a bit unnerving that it may warrant intervention (intubation and ventilation). There’s also been discussion (for a while now) that people may actually do worse with intubation. Now, this is in some regard a stupid observation, because being intubated fundamentally means that you’re sicker than someone who isn’t intubated, but it appeared that there were a number of different variables that did lead to the idea that, all things being equal, people were having worse outcomes with being intubated. Currently, you don’t hear anything about ventilators. As of Friday, one of the largest hospitals in the state had only two people with COVID on ventilators. I’m not 100% certain on what’s going on currently, but there may be more reliance on CPAP, and that was one of the big things they started doing in Italy.
- It’s hard to know how much is how things are counted, as this varies by locality, and to know how much this has changed over time. I don’t know that this would be a significant change in numbers, but I’ve had three patients who would have been considered COVID deaths but that were actively dying (<1 month anticipated) before getting COVID. It will take a while to determine what happened in general, but all-cause mortality for the entire year would need to be looked at when we average this over a calendar year. I don’t know (early on) how many deaths were presumptive based on exposure or anything else that wasn’t a confirmed case.
The biggest takeaway, however, is trying to establish what are norms and what are outliers. If we’re comparing cases curves, all the other European countries are within comparable ranges. Ours is an outlier. When comparing death curves, we aren’t an outlier. So I think the question really needs to be asked is if our low (relative to cases) death curve is an outlier or if the death curve is more true to reality and the plateaued cases curve is the outlier (not saying it’s false, just that there are perhaps more variable outliers making up our numbers than other countries’). If we say that the numbers of cases is a good capture, and that the rest of Europe is getting an equally good capture of numbers in their curves, then it’s essentially suggesting that there’s some kind of magic in the US where we were able to break the death curve and dissociate it from the number of cases. It’s possible, but I don’t find that idea very tenable.
- Most deaths were in nursing homes. There was less lead time initially getting this shut down, and by the time it started spreading it wasn’t able to be contained in those settings as well is it can now. I have my own story regarding this that I’ll share more on when this is all over, but it was a very scary situation going for over a month that I had no relief from.
- In relation to above, people are self-selecting their exposure levels, and if we had more data on the demographics, I’d suspect the age distributions of those infected would trend to lower ages over time.
The biggest takeaway, however, is trying to establish what are norms and what are outliers. If we’re comparing cases curves, all the other European countries are within comparable ranges. Ours is an outlier. When comparing death curves, we aren’t an outlier. So I think the question really needs to be asked is if our low (relative to cases) death curve is an outlier or if the death curve is more true to reality and the plateaued cases curve is the outlier (not saying it’s false, just that there are perhaps more variable outliers making up our numbers than other countries’). If we say that the numbers of cases is a good capture, and that the rest of Europe is getting an equally good capture of numbers in their curves, then it’s essentially suggesting that there’s some kind of magic in the US where we were able to break the death curve and dissociate it from the number of cases. It’s possible, but I don’t find that idea very tenable.
I think these things are lining up a bit. Looking at Spain/Italy as a comparison point almost 70% of there recorded cases were in folks age 50+, we're under 50%. We seem to have done a good job of keeping our elderly from getting it so far.
Sources:
https://www.statista.com/statistics/1103023/coronavirus-cases-distribution-by-age-group-italy/
https://en.wikipedia.org/wiki/Template:COVID-19_pandemic_data/Spain_medical_cases/By_age_and_gender
https://www.cdc.gov/mmwr/volumes/69/wr/mm6924e2.htm
fishonjazz
Well-Known Member
Contributor
2018 Award Winner
2019 Award Winner
20-21 Award Winner
2022 Award Winner
2023 Award Winner
2024 Award Winner
2025 Award Winner
Nope. Maybe you meant nobody except meYes. Is this something you already been hearing elsewhere?

Sent from my ONEPLUS A6013 using JazzFanz mobile app
leftyjace
Well-Known Member
Spoken like a true 20 year old.My point is, you focus on the scary #'s. Not the #'s that are actually relevant. I had corona, I couldn't smell anything for 2 weeks, thats about it. now I understand, extremely fat, old, near death people will have a different experience. I'm sure you'll pull the 1 in 100,000 example out of your *** to try and disprove that but those are the facts. Extremely fat, old, and unhealthy are "supposed" to die when they get a serious sickness. The circle of life if you will.
There is no reason for people to freak out, or go back into lockdown. Wear masks, it did but it didn't save me but hey, I did my best. Now if I was a fat unhealthy old person I would be extremely cautious. But it's not up to everyone else to disrupt their lives and be responsible for me.
Ya know?
Keep pushing the scariest #'s you can find though.
And if that, fat, old, unhealthy person is your grandma or your parents? Are they "supposed" to die?
Handlogten's Heros
Well-Known Member
2019 Award Winner
20-21 Award Winner
2022 Award Winner
2023 Award Winner
2024 Award Winner
2025 Award Winner
2025 Prediction Contest Winner
View attachment 9484
Another low today of 267. Lowest since March 23, three months ago. Again, you can say this is a weekend, but there have been 26 weekend days since then with none of them being that low. Tomorrow’s numbers will again be lower before ticking up a little bit Tuesday.
Obviously, one could appeal to the past few days having increased cases. However, the deaths have continued to steadily decline for the past two months, independent of the fact that incidence of new cases hasn’t dropped. While we’ve had higher numbers the past few days, we’ve also set daily records for the quantity of tests administered, and the US is testing more than anyone else is. True, our curve with relation to new cases looks worse than other countries’, but our death curves look the exact same as all those other countries.
But nobody’s talking about that.
I think there have been some that said it really isn't fair to compare us to other smaller countries. We are like a small group of countries so some areas are rising, some falling, etc.
You did a good job at breaking down the death rate curve in a post below... I think part of it is we are/will get better at treating it... as you know doctors "practice" medicine. Read some stories that said steroids were helping, read one that said a heartburn medication showed some promise in helping (it was a super limited sample).
My wife is really fed up with sheltering in place... she's told me she just wants to get it and be done with it... I've told her there are a lot of issues with that, but even if we just delay the inevitable that there would be better treatments available the longer you can delay infection. She's not really serious... just frustrated... she is not a homebody.
Handlogten's Heros
Well-Known Member
2019 Award Winner
20-21 Award Winner
2022 Award Winner
2023 Award Winner
2024 Award Winner
2025 Award Winner
2025 Prediction Contest Winner
This may be my fault. I planned a trip to Utah for end of July that looks like it will get canceled. The virus doesn't want me to go back I guess.
Beer
Well-Known Member
This may be my fault. I planned a trip to Utah for end of July that looks like it will get canceled. The virus doesn't want me to go back I guess.
Don't fret. Won't happen. The idiot SLC mayor might try and pull some bs but she should be the only one.
